Organ-On-Chip Devices Show Promise In Drug Discovery
By Adam Nightingale, senior mechanical engineer, Springboard Pro
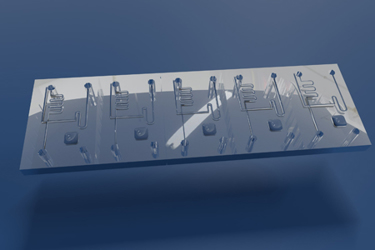
There is growing interest in the potential uses for organ-on-chip devices as a novel tool for drug discovery. These devices offer a unique platform that mimics the physiology and function of human organs, providing a more accurate representation of human biology than traditional cell culture systems. They are microfluidic systems consisting of a small 3D microscale chip with channels and chambers that are lined with living human cells. The cells are grown in a manner that allows them to interact with each other, creating an environment that mimics the physiology and function of the targeted organ. In this article, I’ll describe how they work and their role in drug discovery.
How Do Organ-On-Chip Devices Work?
Organ-on-chip devices work by recreating the microenvironment of specific human organs in vitro. They typically consist of two primary components: the microfluidic chip and the living cells. The chip is designed to provide a 3D scaffold for the cells, allowing them to grow in a manner that is similar to their natural environment. The cells are then seeded onto the chip and cultured in a microfluidic system that provides them with the necessary nutrients and oxygen.
The microfluidic system also allows researchers to control the flow of fluids and chemicals within the chip, simulating the physiological conditions of the targeted organ. This allows researchers to study how drugs and other compounds interact with the cells in a more accurate and realistic manner than traditional cell cultures. These microfluidic systems might be channel microfluidics, droplet-based microfluidics technologies, or plate-based.
In addition to organ-on-chip devices based on traditional microfluidics, even more advanced models are being developed. These models are known collectively as “microphysiological systems,” or MPS, and include tumoroids and organoids. Tumoroids are miniature models of tumors grown from patient-derived cells. These tumoroids mimic the complex cellular interactions and heterogeneity of actual tumors, making them a powerful tool for drug screening and personalized medicine. Likewise, organoids, grown from stem cells to mimic specific human organs, can replicate the complex structure and function of actual organs, including the inclusion of multiple cell types and even vasculature and movements such as a heartbeat. This allows researchers to study the development and function of organs in vitro, providing a better understanding of disease and potential treatments. A good example of this is Swiss company inSphero and its spheroid 3D microtissues, which are already shedding light on treatment of liver diseases such as non-alcoholic steatohepatitis (NASH).
What Is The Role Of Organ-On-Chip Devices In Drug Discovery?
Organ-on-chip devices have the potential to revolutionize drug discovery by providing a more accurate representation of human biology. Traditional cell culture systems are limited in their ability to mimic the complex microenvironment of human organs, in particular the complex interactions between different organs in the body. This makes it difficult to accurately predict how drugs and other compounds will behave in the human body.
Testing in animals such as mice has long been the most common way of testing whether new drugs are safe prior to human clinical trials. Due to the significant biological differences from humans, animal testing is a poor predictor of drug efficacy. Better predicting drug efficacy at earlier stages of the development process has the potential to massively increase the productivity of new drug development – as many as 85% of early clinical trials for novel drugs fail to become approved for clinical use. For novel cancer drugs, studies have shown that less than 8% of trials successfully translate from animal models to clinical trials.1
The use of organ-on-chip models in drug discovery may not be far away. German pharmaceutical company Merck stated in 2021 that it is its “long-term aspiration to be a pioneer in phasing out animal use and replacing animal work by better, cutting edge alternatives,”2 although a timeline for this has not been set. Since 2017, the FDA has been collaborating with the Wyss Institute at Harvard University to evaluate the use of organ-on-chip technologies for toxicity testing, and in January the FDA Modernization Act 2.0 was signed into U.S. law to encourage ”innovation and get safer, more effective drugs to market more quickly” by moving away from animal testing.
The company Emulate, based in Boston, MA, has attracted significant funding (approx. USD $224M to date) with its Human Emulation System. This system uses an instrument with disposable chips to model tissue from the kidney, lung, liver, and even brain in one in vitro environment. Another high-profile company in this area, TARA Biosystems, was acquired by Valo Health in April 2022. Valo is looking to leverage TARA’s human cardiac tissue models with its proprietary Opal artificial intelligence platform to discover the next generation of cardiovascular disease drugs.
In addition to providing better reliability than animal models, organ-on-chip devices could offer a platform for innovative therapies such as personalized medicine based on human cells and genes. By using a patient's own cells to create an organ-on-chip model, researchers can study how drugs and other compounds will affect that specific individual, providing a more personalized approach to drug development and treatment.
Another potentially significant field where organ-on-chip technology may play a role is in the study of rare diseases. These diseases often cannot be studied in animals at all, and it is estimated that of the approximately 7,000 of these rare disease that have been identified, only 400 are actively studied.3 Companies such as Hesperos Inc. in Orlando, FL, are working toward a full “human-on-chip” model suitable for studying these rare diseases, and it recently partnered with Sanofi to get FDA approval for a clinical trial with an existing drug to extend its use to treat the rare autoimmune condition chronic inflammatory demyelinating polyneuropathy, or CIDP.
Conclusion
Organ-on-chip devices offer a promising new tool for drug discovery. By mimicking the physiology and function of human organs, these devices provide a more accurate representation of human biology than traditional animal models or cell culture systems. This can help to identify potential side effects due to organ interaction and test for efficacy earlier in the drug development process, ultimately reducing the time and cost of drug development. Organ-on-chip devices also offer a platform for innovative medicine and cell and gene therapies, providing a more personalized approach to drug development and treatment. As the technology continues to develop, we can expect to see organ-on-chip devices become an increasingly important tool in drug discovery and personalized medicine.
References
- Mak, I. W., Evaniew, N., & Ghert, M. (2014). Lost in translation: animal models and clinical trials in cancer treatment. American Journal of Tranlsational Research.
- Merck. (2021). Merck Sustainability Report 2021.
- Rumsey, J. W., & Hickman, J. J. (2022). Classical Complement Pathway Inhibition in a “Human-On-A-Chip” Model of Autoimmune Demyelinating Neuropathies. Advanced Therapeutics.
About The Author:
 Adam Nightingale is a Chartered Mechanical Engineer and works as principal engineer at Springboard Pro. With a background in microfluidics and an M.Eng. in manufacturing engineering from the University of Cambridge, he has a broad range of experience from consulting to startups, all within the medical and life sciences fields. He has taken lab-on-chip products from early-stage R&D all the way through to high-volume production.
Adam Nightingale is a Chartered Mechanical Engineer and works as principal engineer at Springboard Pro. With a background in microfluidics and an M.Eng. in manufacturing engineering from the University of Cambridge, he has a broad range of experience from consulting to startups, all within the medical and life sciences fields. He has taken lab-on-chip products from early-stage R&D all the way through to high-volume production.
